Review
, Volume: 12( 1)Is the Cannabidiol Potentially Useful for the Treatment of Neuropsychiatric and Drug-Use Disorders?
- *Correspondence:
- Manzanares J , Institute of Neurosciences, Miguel Hernández-CSIC University, Avda de Ramón y Cajal s/n, San Juan de Alicante, Alicante, Spain, Tel: +34965233700; E-mail: jmanzanares@goumh.umh.es.
Received: December 20, 2016; Accepted: January 16, 2017; Published: January 23, 2017
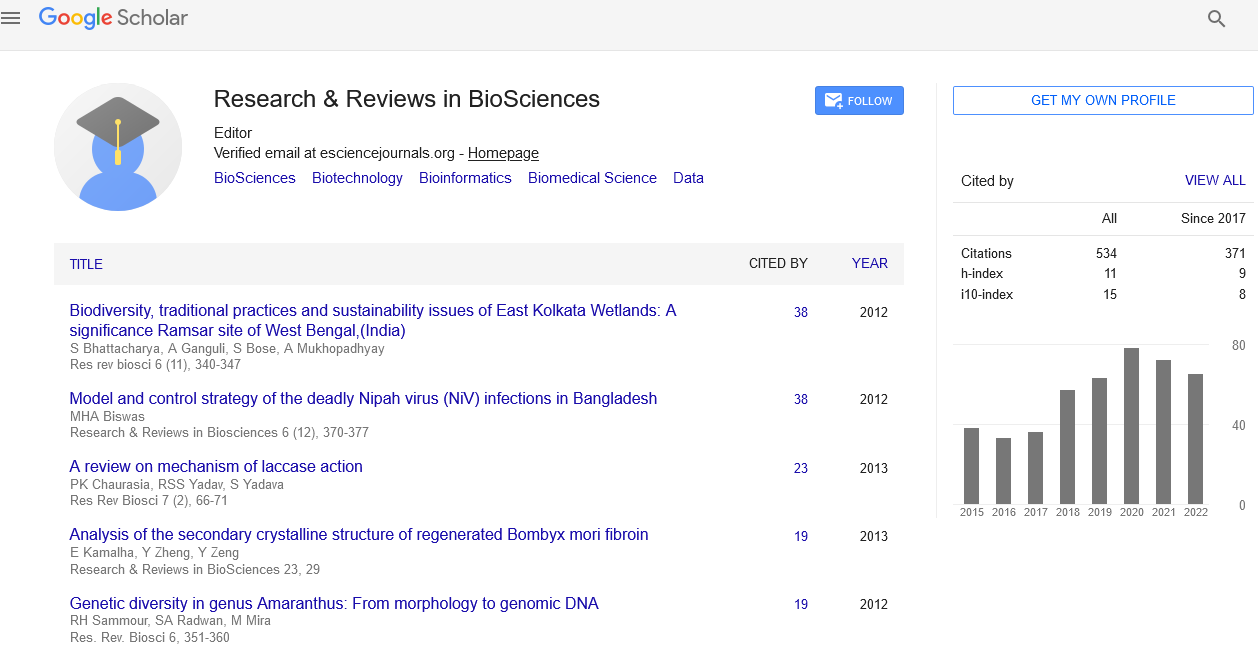
Citation: Manzanares J and García-Gutiérrez MS. Is the Cannabidiol Potentially Useful for the Treatment of Neuropsychiatric and Drug-Use Disorders. Res Rev Biosci. 2017;12(1):112.
Abstract
Preclinical and clinical evidence collected over the past years suggests that Cannabidiol (CBD), one of the main compounds of the plant Cannabis sativa, presents potential therapeutic activity for the treatment of neuropsychiatric and drug-use disorders. Studies carried out in animal models revealed that CBD presents anxiolytic-like effects in different paradigms such as the Vogel conflict test [1], the elevated plus maze test [2] and the fear conditioning test [3-6]. Antidepressant-like effects were reported in mice following acute or repeated CBD administration in the forced swim [7] and in the tail suspension tests [8]. In addition, CBD decreased defensive behaviors evoked by predator exposure, a proposed model of panic attacks and posttraumatic stress disorder (PTSD) [9,10]. Interestingly, CBD reversed the alteration of prepulse inhibition (PPI) observed in spontaneously hypertensive rats [11] and in a glutamate-based models of psychosis [12] and exhibited a similar profile compared with atypical antipsychotic drugs [13,14]. Indeed, CBD improved cognition in several preclinical models of cognitive impairment [15]. Recent evidences pointed out that CBD might be a potential treatment for drug-use disorders. CBD reduced heroin craving and relapse [16], and cocaine [17] and alcohol consumption mice [18]. In clinical studies, CBD reduced anxiety and the psychotic-like symptoms induced by Δ9-tetrahydrocannabinol (ï„9-THC) [19]. Indeed, CBD reduced anxiety in healthy volunteers [20-22], in treatment-naïve social phobic patients [23] and in posttraumatic stress disorder [24]. Also, CBD reduced the psychotic symptoms in schizophrenia [25,26] and in Parkinson´s disease [27,28].
Commentary
Preclinical and clinical evidence collected over the past years suggests that Cannabidiol (CBD), one of the main compounds of the plant Cannabis sativa, presents potential therapeutic activity for the treatment of neuropsychiatric and drug-use disorders.
Studies carried out in animal models revealed that CBD presents anxiolytic-like effects in different paradigms such as the Vogel conflict test [1], the elevated plus maze test [2] and the fear conditioning test [3-6]. Antidepressant-like effects were reported in mice following acute or repeated CBD administration in the forced swim [7] and in the tail suspension tests [8]. In addition, CBD decreased defensive behaviors evoked by predator exposure, a proposed model of panic attacks and posttraumatic stress disorder (PTSD) [9,10]. Interestingly, CBD reversed the alteration of prepulse inhibition (PPI) observed in spontaneously hypertensive rats [11] and in a glutamate-based models of psychosis [12] and exhibited a similar profile compared with atypical antipsychotic drugs [13,14]. Indeed, CBD improved cognition in several preclinical models of cognitive impairment [15]. Recent evidences pointed out that CBD might be a potential treatment for drug-use disorders. CBD reduced heroin craving and relapse [16], and cocaine [17] and alcohol consumption mice [18].
In clinical studies, CBD reduced anxiety and the psychotic-like symptoms induced by Δ9-tetrahydrocannabinol (Δ9-THC) [19]. Indeed, CBD reduced anxiety in healthy volunteers [20-22], in treatment-naïve social phobic patients [23] and in posttraumatic stress disorder [24]. Also, CBD reduced the psychotic symptoms in schizophrenia [25,26] and in Parkinson´s disease [27,28].
In spite of the number of findings suggesting the potential therapeutic use of CBD, there is some controversy regarding its profile as a drug of abuse that significantly hampers further development of basic and clinical studies. CBD is currently classified in the Schedule 1 according to United Nations Single Convention on Narcotic Drugs of 1961 Comprehensive Drug Abuse Prevention and Control Act) of United States (US) [29]. A schedule I controlled substance is defined by the controlled substances act (CSA) as a substance presenting “no currently accepted medical use, a lack of accepted safety for the use under medical supervision, and a high potential for abuse”. Furthermore, CBD is classified as a Schedule 2 drug according to the Controlled Drugs and Substances Act [29] also inferring “a high potential for abuse which may lead to severe psychological or physical dependence”. However, there is no evidence that supports these considerations. On the other hand, CBD is not under any special restrictions in Europe. In contrast to THC, CBD did not induce euphoria or intoxication [30-32]. The lack of psychoactive activity appears to be related with its low affinity on CB1 receptors (100 fold less than THC) [33]. Interestingly, recent studies carried out in our laboratory demonstrated that CBD did not induce conditioned-place preference, withdrawal signs or oral self-administration suggesting lack of properties as a drug of abuse [34].
To date, no significant side effects have been observed in any of the preclinical and clinical studies carried out with CBD. Furthermore, CBD is present in Nabiximols (marketed as Sativex) currently approved for the treatment of spasticity in multiple sclerosis in several countries in Europe. Therefore, there is a large body of information regarding its safety and side effects.
Taken together, these results suggest that the classification of CBD in the Schedule I should be revised. The reconsideration of CBD as a drug lacking potential for drug abuse would allow the development of basic and clinical studies needed to elucidate its potential therapeutic use for the treatment of neuropsychiatric diseases.
Acknowledgments
This research was supported by “Instituto de Salud Carlos III” (RETICS, RD12/0028/0019), “Plan Nacional Sobre Drogas” (PNSD 2016/016) and “Ministerio de Economía y Competitividad” (FIS, PI14/00438) Grants to J Manzanares.
Conflict of Interest
Authors state that they have no biomedical financial interest or potential conflicts of interest.
References
- Moreira FA, Aguiar DC, Guimaraes FS. Anxiolytic-like effect of cannabidiol in the rat Vogel conflict test. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:1466-71
- Guimaraes FS, Chiaretti TM, Graeff FG, et al. Antianxiety effect of cannabidiol in the elevated plus-maze. Psychopharmacology. 1990;100:558-9.
- Lemos JI, Resstel LB, Guimaraes FS. Involvement of the prelimbic prefrontal cortex on cannabidiol-induced attenuation of contextual conditioned fear in rats. Behav brain res. 2010;207:105-11.
- Resstel LB, Joca SR, Moreira FA, et al. Effects of cannabidiol and diazepam on behavioral and cardiovascular responses induced by contextual conditioned fear in rats. Behav brain res. 2006;172:294-8.
- Norris C, Loureiro M, Kramar C, et al. Cannabidiol modulates fear memory formation through interactions with serotonergic transmission in the mesolimbic system. Neuropsychopharmacology. 2016;41:2839-50.
- Blessing EM, Steenkamp MM, Manzanares J, Marmar CR. Cannabidiol as a Potential Treatment for Anxiety Disorders. Neurotherapeutics. 2015;12:825-36.
- Zanelati TV, Biojone C, Moreira FA. Antidepressant-like effects of cannabidiol in mice: Possible involvement of 5-HT1A receptors. Br jpharmacol. 2010;159:122-8.
- Schiavon AP, Bonato JM, Milani H, et al. Weffort de Oliveira RM;Influence of single and repeated cannabidiol administration on emotional behavior and markers of cell proliferation and neurogenesis in non-stressed mice. Prog Neuropsychopharmacol Biol Psychiatry. 2015;64:27-34.
- Campos AC, Ferreira FR, Guimaraes FS. Cannabidiol blocks long-lasting behavioral consequences of predator threat stress: possible involvement of 5HT1A receptors. J psychiatr res. 2012;46:1501-10.
- Uribe-Marino A, Francisco A, Castiblanco-Urbina MA, et al. Anti-aversive effects of cannabidiol on innate fear-induced behaviors evoked by an ethological model of panic attacks based on a prey vs the wild snake Epicrates cenchria crassus confrontation paradigm, Neuropsychopharmacology. 2012;37:412-21.
- Peres FF, Levin R, Almeida V, et al. Cannabidiol, among Other Cannabinoid Drugs, Modulates Prepulse Inhibition of Startle in the SHR Animal Model:Implications for Schizophrenia Pharmacotherapy. Front Pharmacol. 2016;7:303.
- Long LE, Malone DT, Taylor DA. Cannabidiol reverses MK-801-induced disruption of prepulse inhibition in mice. Neuropsychopharmacology. 2006;31:795-803.
- Moreira FA, Guimaraes FS. Cannabidiol inhibits the hyperlocomotion induced by psychotomimetic drugs in mice. Eur J pharmacol. 2005;512:199-205.
- Zuardi AW, Rodrigues JA, Cunha JM. Effects of cannabidiol in animal models predictive of antipsychotic activity. Psychopharmacology. 1991;104:260-64
- Osborne AL, Solowij N, Weston-Green K. A systematic review of the effect of cannabidiol on cognitive function: Relevance to schizophrenia. Neurosci Biobehav Rev. 2017;72:310-24.
- Ren Y, Whittard J, Higuera-Matas A, et al. Cannabidiol, a nonpsychotropic component of cannabis, inhibits cue-induced heroin seeking and normalizes discrete mesolimbic neuronal disturbances. J Neurosci. 2009;29:14764-69.
- Weiss F, Laque A, Wagner G, et al. Transdermal CBD attenuates cocaine intake in rats with addiction-linked cocaine history. Annual Meeting Society for Neuroscience. San Diego (CA). 2016.
- Viudez-Martinez A, Garcia-Gutierrez MS, Navarron C, et al. Cannabidiol mediated regulation of alcohol consumption. Addict Biol. Forthcoming 2016.
- Zuardi AW, Shirakawa I, Finkelfarb E, et al. Action of cannabidiol on the anxiety and other effects produced by delta 9-THC in normal subjects. Psychopharmacology. 1982;76:245-50.
- Zuardi AW, Cosme RA, Graeff FG, et al. Effects of ipsapirone and cannabidiol on human experimental anxiety. J Psychopharmacol. 1993;7:82-8.
- Crippa JA, Zuardi JA, Garrido GE, et al. Effects of cannabidiol (CBD) on regional cerebral blood flow. Neuropsychopharmacology. 2004;29:417-26
- Soares VP, Campos AC. Evidences for the anti-panic actions of Cannabidiol. Curr Neuropharmacol.Forthcoming 2016
- Bergamaschi MM, Queiroz RH, Chagas MH, et al. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology. 2011;36:1219-26.
- Shannon S, Opila-Lehman J. Effectiveness of Cannabidiol oil for pediatric anxiety and insomnia as part of posttraumatic stress disorder:A case report. Permanente J. 2016;20:108-111.
- Zuardi AW, Morais SL, Guimaraes FS, et al. Antipsychotic effect of cannabidiol. J clin psychiatry. 1995;56:485-486.
- Leweke FM, Piomelli D, Pahlisch F, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2:94.
- Zuardi AW, Crippa JA, Hallak JE, et al.Cannabidiol for the treatment of psychosis in Parkinson's disease.J Psychopharmacol. 2009;23:979-83.
- CSA: Comprehensive drug use prevention and control act of 1970. FDA US Food and Drug Administration. (1970).
- Ministry of Justice C: Hashish-I. Tetrahedron. 1963;19
- Martin-Santos R, Crippa JA, Batalla A, et al. Acute effects of a single, oral dose of d9-tetrahydrocannabinol (THC) and cannabidiol (CBD) administration in healthy volunteers. Curr Pharm Des. 2012;18:4966-79
- Fusar-Poli P, Crippa JA, Bhattacharyya S, et al. Distinct effects of {delta}9-tetrahydrocannabinol and cannabidiol on neural activation during emotional processing.Arch gen psychiatry. 2009;66:95-105.
- Winton-Brown TT, Allen P, Bhattacharyya S, et al. Modulation of auditory and visual processing by delta-9-tetrahydrocannabinol and cannabidiol: an FMRI study. Neuropsychopharmacology. 2011;36:1340-8
- Zlebnik NE, Cheer JF. Beyond the CB1 Receptor: Is Cannabidiol the Answer for Disorders of Motivation? Ann rev neurosci. 2016;39:1-17